Managing payer contracts with spreadsheets puts healthcare providers at a significant disadvantage—like trying to navigate complex terrain with an outdated map. While reimbursement models evolve with mounting complexity and margins continue to shrink, healthcare organizations require sophisticated contract management solutions designed specifically for their unique challenges.
The evolving challenge of payer contracts
The relationship between providers and payers forms the financial backbone of healthcare delivery in America. Yet, many organizations still rely on outdated methods to manage these critical relationships.
The high cost of outdated methods
Traditional contract management approaches like manual tracking, scattered documents and disconnected spreadsheets leave providers vulnerable to revenue leakage and compliance issues. With many contracts representing millions in potential revenue, healthcare organizations cannot afford these inefficiencies.
Today’s unique contracting landscape
Today, medical providers face unique contracting challenges:
- Managing hundreds of distinct payer contracts, each with unique terms
- Tracking complex reimbursement models across multiple service lines
- Navigating constantly changing regulatory requirements
- Ensuring compliance with intricate contract terms
- Preparing for contract negotiations with data-backed strategies
Given these complexities, let’s explore why specialized healthcare contract management software has become essential for organizational sustainability and financial health.
What is contract management in healthcare?
At its core, it’s the systematic oversight of agreements between providers and payers. This encompasses everything from initial negotiation to execution, monitoring, and renewal.
The contract management process in healthcare involves:
- Contract creation and negotiation
- Digital storage and organization
- Continuous monitoring and compliance tracking
- Performance analysis against benchmarks
- Strategic contract renewal planning and renegotiation
Unlike generic business contracts, insurance contracts contain complex reimbursement structures, quality metrics, regulatory considerations, and patient care standards that directly impact an organization’s financial health and clinical operations.
The true cost of inadequate contract management
The stakes are particularly high in healthcare contract management. Studies show that inefficient contract management systems can cost organizations 3-5% of their annual revenue through missed opportunities, undetected underpayments, and unmonitored contract terms.
Common revenue leakage in healthcare scenarios
Consider these common scenarios:
- A hospital fails to notice when a payer doesn’t implement negotiated rate increases, losing hundreds of thousands in legitimate revenue
- A medical practice unknowingly continues operating under expired contract terms instead of newly negotiated rates
- Your practice administrator lacks visibility into which contracts are underperforming, making strategic planning impossible
- Teams spend countless hours manually extracting and analyzing data that could be automated
As one healthcare CFO noted in industry reports, “We discovered we were losing over $1 million annually simply because we couldn’t effectively monitor all our contract terms across dozens of payers.”
This reality is driving more organizations toward specialized solutions that address these unique healthcare challenges.
Healthcare-specific contract management: Why generic solutions fall short
Healthcare organizations face unique challenges that demand specialized tools. Generic contract management solutions simply aren’t designed to handle:
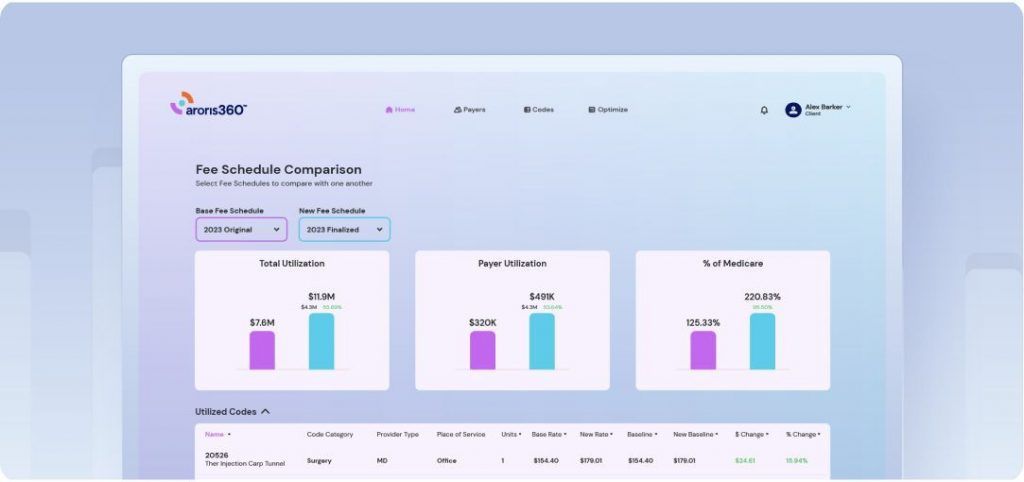
1. Complex reimbursement models
Insurance contracts establish intricate methodologies for determining payment. From fee schedules and carve-outs to value-based care arrangements, healthcare reimbursement requires specialized analysis capabilities that most software can’t deliver.
An effective healthcare contract management system must:
- Store and interpret complex fee schedules with multiple variables
- Model various reimbursement scenarios based on service mix and volume
- Compare performance across different contract structures and payers
- Identify outliers and opportunities for improvement in specific service lines
2. Regulatory compliance requirements
Payer contracting operates under strict regulatory oversight. Your management platform must incorporate compliance features specific to HIPAA, Stark Law, Anti-Kickback Statute, and constantly evolving payer requirements.
3. Revenue cycle dependencies
Unlike other industries, healthcare’s contractual terms directly impact day-to-day operations—from charge capture and coding to claims submission and denial management. The most effective solutions connect contract terms with revenue cycle operations to ensure consistent execution.
4. Negotiation complexity
Healthcare payer contract negotiation involves complex trade-offs between reimbursement models, patient access, network participation, and quality incentives. Effective solutions provide negotiation intelligence based on historical performance, market benchmarks, and payer behavior patterns.
When evaluating solutions, these healthcare-specific capabilities should be non-negotiable requirements.
Essential components of effective healthcare contract management software
Purpose-built solutions transform how you manage payer relationships through these critical capabilities:

1. Centralized digital repository
Create a single source of truth that eliminates lost documents, maintains version control, and provides authorized access from anywhere. This centralization helps teams find critical contract language when responding to payer inquiries or preparing for negotiations.
2. Proactive monitoring system
Implement automated alerts for key dates, performance thresholds, and contract milestones. This preventative approach ensures you never miss deadlines for renegotiation windows, amendments, or termination notices—all of which have significant revenue implications.
3. Comprehensive performance analytics
Deploy tools that track actual reimbursements against contracted rates at the service line level. Advanced solutions can identify systematic underpayments, monitor payer adherence to contract terms, and quantify the financial impact of specific contract clauses.
4. Intelligent workflow automation
Replace manual processes with automated approval pathways, contract generation, and compliance verification. Workflow automation reduces processing time, eliminates bottlenecks, and creates audit trails that improve accountability.
5. Healthcare ecosystem integration
Connect your contract management solution with your EHR, billing systems, and other platforms for a cohesive operational environment. This integration enables real-time validation of contract terms during patient registration, claims processing, and financial reporting.
Measurable outcomes: The ROI of specialized contract management
Organizations implementing healthcare-specific contract management systems consistently report:
- Increase in net revenue through systematic identification and correction of underpayments, often translating to millions in recovered revenue annually
- More favorable contract terms by leveraging data-driven insights during payer negotiations, including targeted improvements in high-volume service lines
- 30-50% reduction in administrative time spent on contract management tasks, allowing staff to focus on strategic priorities rather than document retrieval and manual tracking
- Significantly reduced compliance risk through consistent documentation, automated monitoring of regulatory requirements, and clear audit trails
- Enhanced strategic planning enabled by comprehensive visibility across the entire contract portfolio, supporting more informed decisions about network participation and service line development
- Improved cash flow through faster contract execution, more accurate claims submission, and reduced payment delays
By investing in purpose-built contract management technology, healthcare organizations establish a foundation for sustainable financial performance in an increasingly complex reimbursement environment.
Select the right solution for your organization
When evaluating contract management software, healthcare organizations should consider:
1. Healthcare-specific expertise
The best healthcare contract management companies bring deep industry knowledge beyond just software features. Evaluate whether your vendor truly understands the nuances of payer contracts, reimbursement models, and regulatory requirements specific to healthcare.
2. Implementation support
What level of assistance is provided during setup and data migration? The transition period is critical for maintaining continuity in your revenue cycle.
3. Integration capabilities
Can the solution connect with existing clinical and financial systems? Seamless integration prevents data silos and ensures consistent information across platforms.
4. Scalability
Will the platform grow with your organization? Consider whether the solution can accommodate additional specialties, locations, or contract volumes as your practice expands.
5. Ongoing support
What training and support are available after implementation, and during payer negotiation phases? Ongoing partnership is essential for maximizing the value of your investment.
From administrative burden to strategic asset
As healthcare organizations and medical practices face unprecedented financial pressures, payer contract management has transformed from a back-office function to a strategic imperative. By implementing specialized solutions designed for healthcare’s unique challenges, organizations can turn document administration from a reactive, paper-shuffling exercise into a proactive revenue optimization strategy.
The right system doesn’t just organize documents—it provides actionable intelligence that drives financial performance and operational excellence.
Securing your financial future
In an era where every dollar counts and payer relationships grow increasingly complex, healthcare organizations can no longer afford to manage their most valuable contracts with outdated tools. Purpose-built contract management platforms don’t just protect your existing revenue—they systematically identify opportunities to optimize it.
The question isn’t whether you can afford to invest in specialized contract management; it’s whether you can afford not to when your competitors are already gaining the advantage. Your organization’s financial sustainability may depend on how you answer.