Contract language review
Our legal experts identify unfavorable clauses in health insurance contracts that limit your revenue potential. We transform complex payer terms into visual data models that pinpoint improvement opportunities.
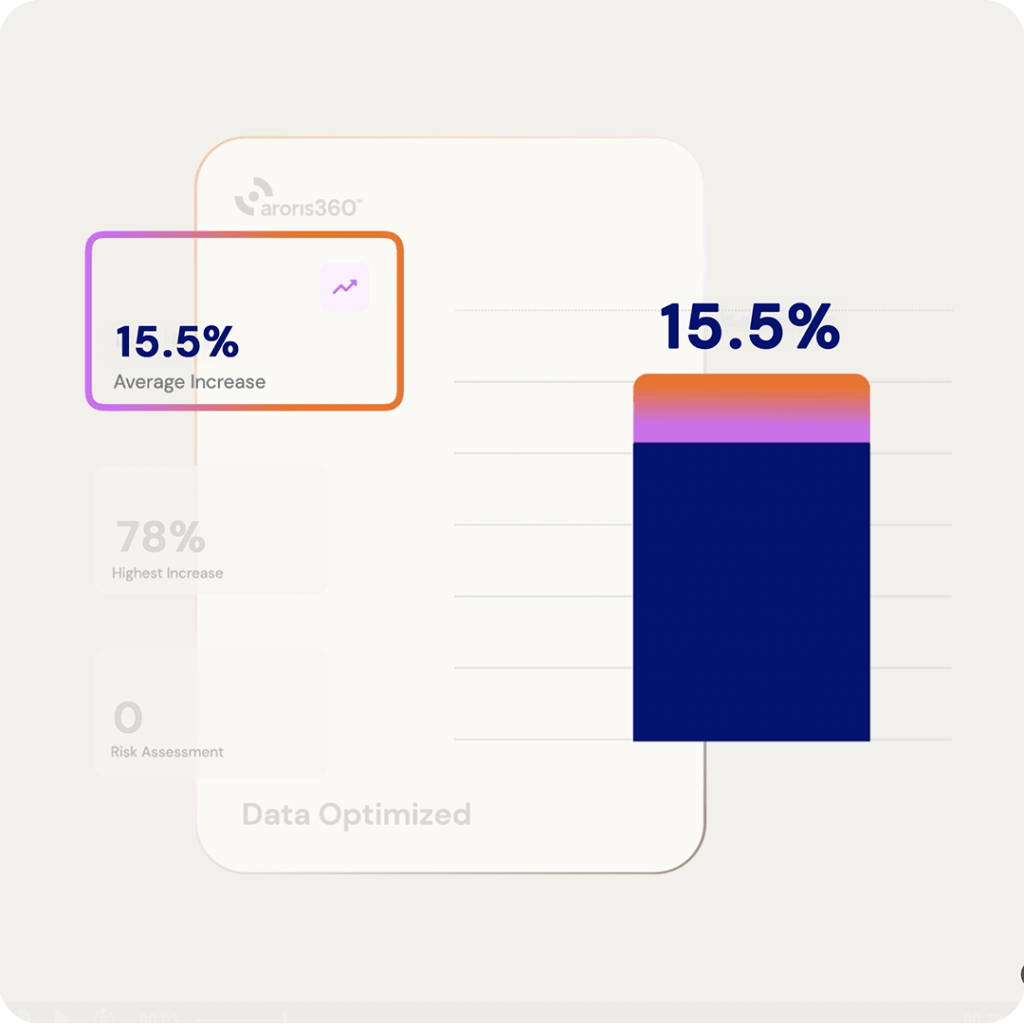
Real Impact:
One client discovered a hidden clause allowing their payer to reduce rates without notice—resulting in a 15% revenue decrease that went undetected for months.
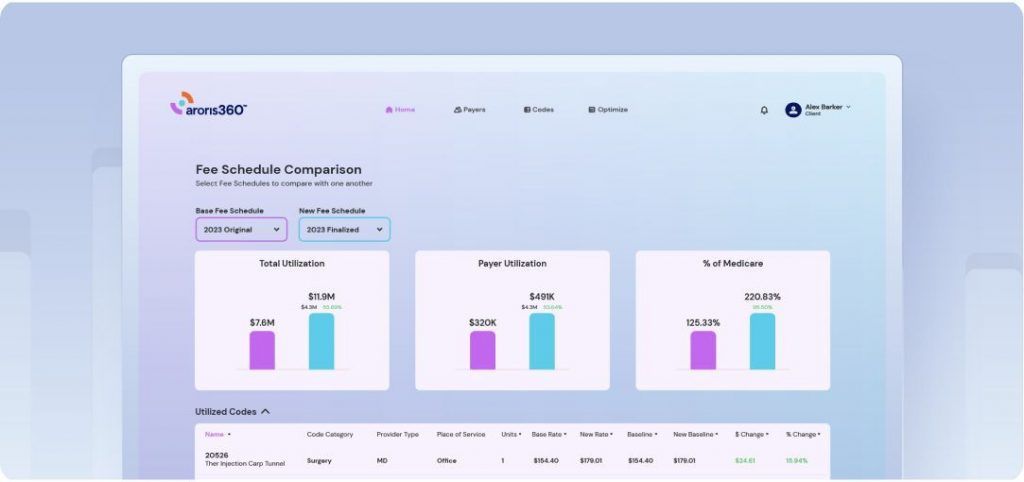
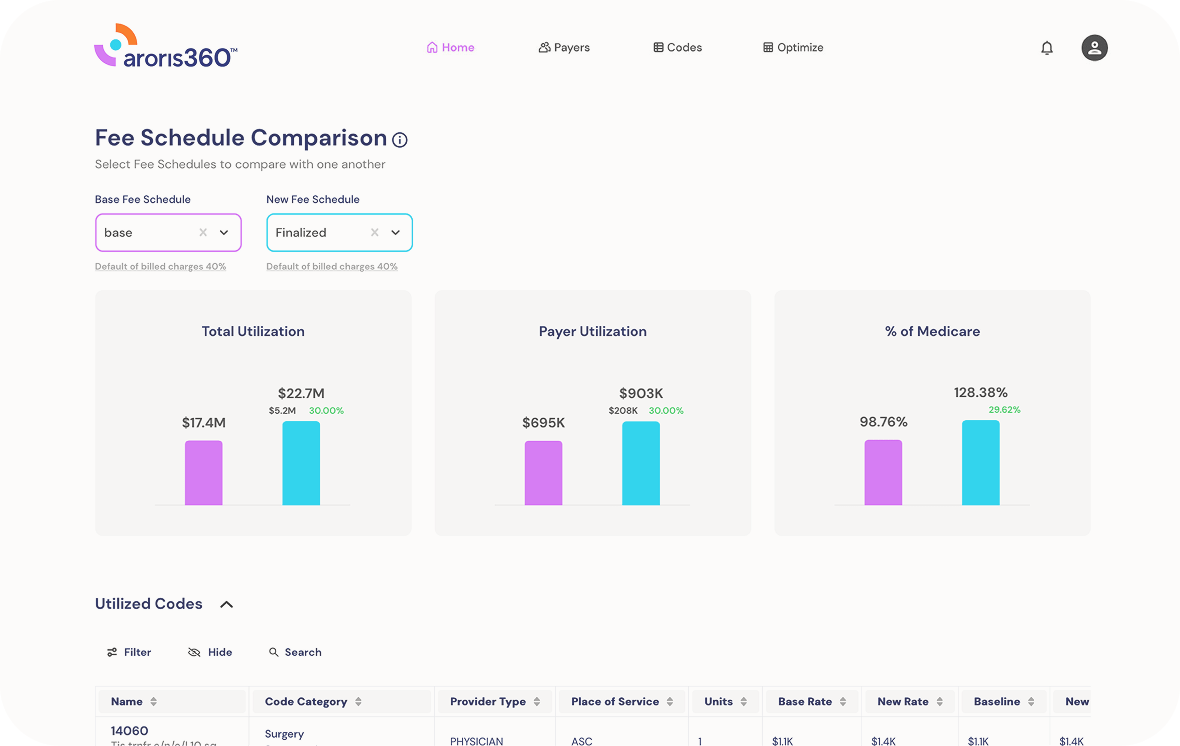
Fee schedule analysis
We analyze every CPT code and corresponding fee to uncover revenue opportunities by:
- Identifying key billing patterns and volume by code
- Detecting payment variances from agreed terms
- Calculating financial impact for each discrepancy
Real Impact:
For a Northeast orthopedic group, our analysis revealed just five codes represented over 60% of their commercial revenue, creating clear
negotiation targets.
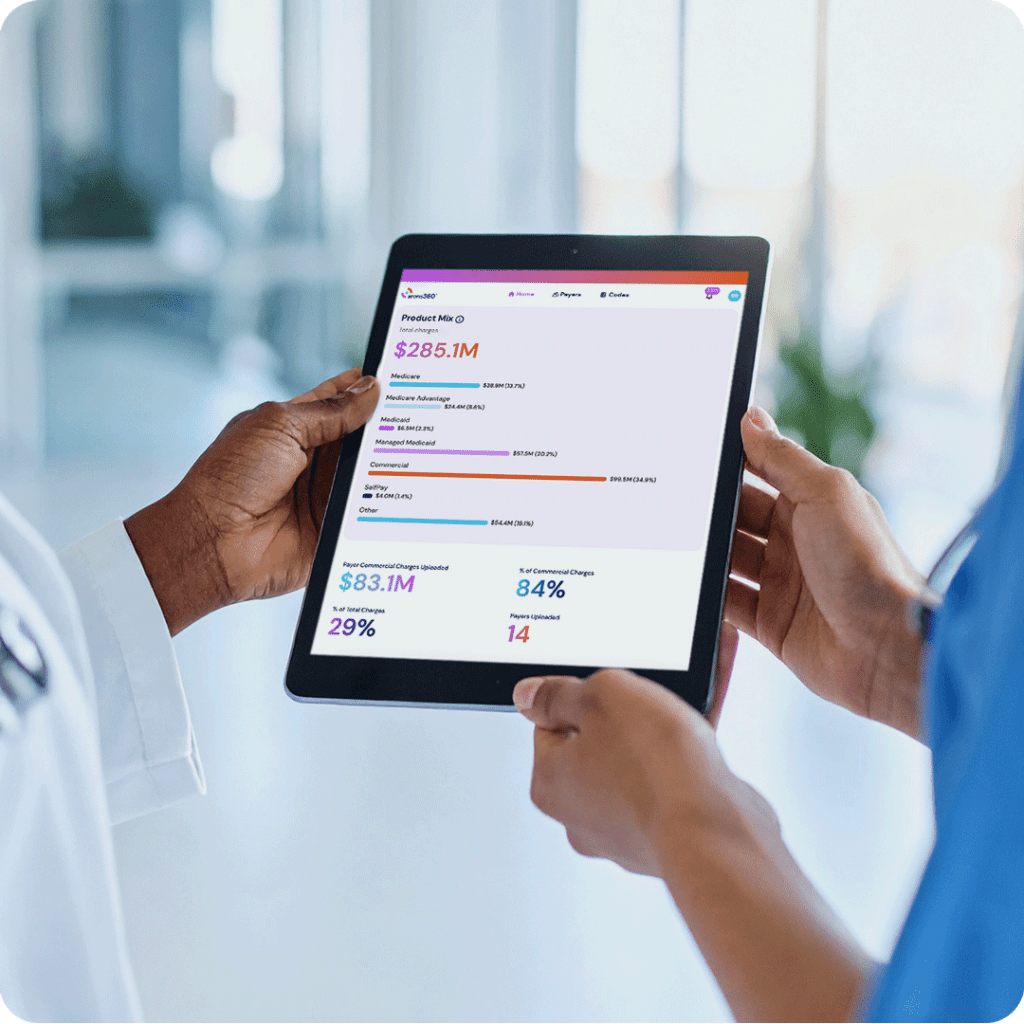
Network participation review
Maximize your market leverage with our comprehensive network analysis:
- In-network vs. out-of-network opportunity evaluation
- Market saturation assessment for your specialty
- Patient steerage pattern analysis
- Identification of exclusive and preferred network opportunities
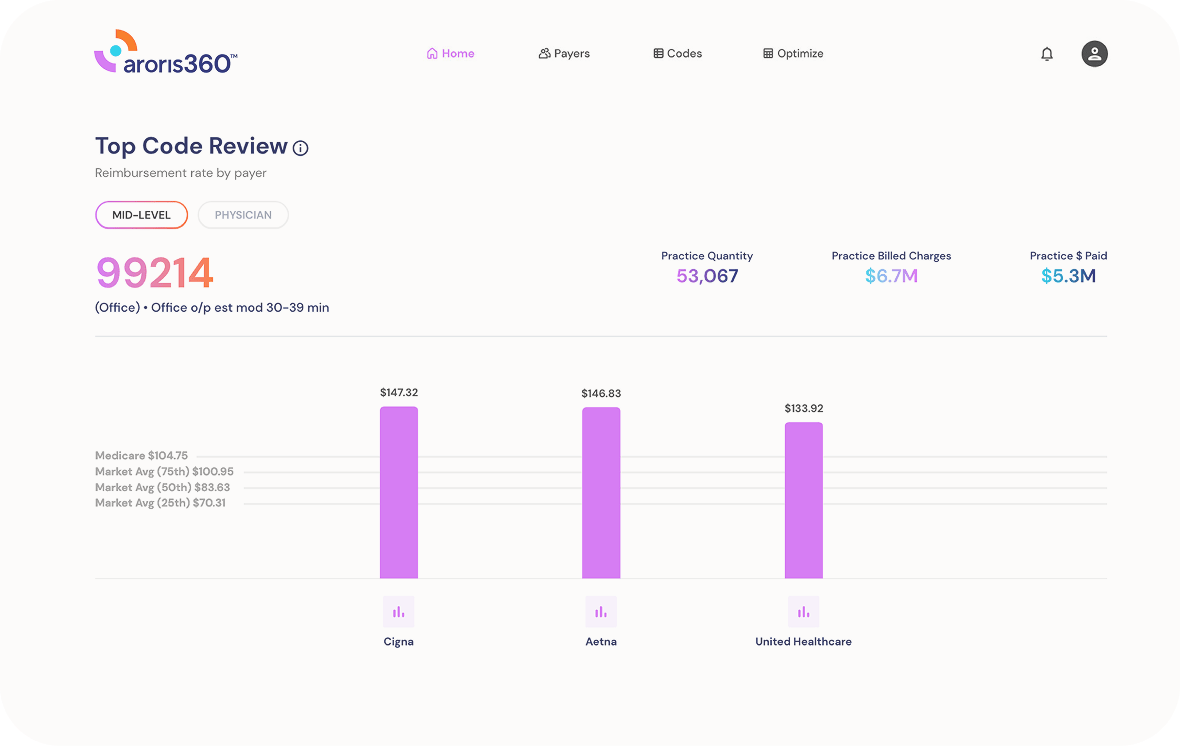
Rate case building
We create compelling fact-based cases for rate increases using:
- Data visualizations that demonstrate payment disparities
- Market-based justifications for increases
- Counter-proposals with specific revenue impacts
- Documentation of quality metrics and your unique value
- Competitive landscape mapping that highlights fee schedule disparities