Understanding medical reimbursement and coding is not just about getting bills paid, but also about creating a data foundation that makes contract optimization possible is essential. For healthcare practices navigating payer negotiations, coding accuracy directly impacts both immediate revenue capture and long-term negotiating power.
The Question Most Practices Don’t Ask
When was the last time you reviewed your coding accuracy before attempting to negotiate higher reimbursement rates?
Most practice administrators focus on rate benchmarking, market data, and competitor comparisons when preparing for payer negotiations. These matter. But here’s a question that rarely gets asked: Is your coding data reliable enough to support your negotiation case?
If you can’t answer that confidently, you may be negotiating from a position of weakness without realizing it.
Why Coding Accuracy Matters Beyond the Claim
Most practice administrators know that coding errors cause claim denials. Medical practices face upwards of $20 billion per year in delayed or lost reimbursements because of denial management costs, with 68% of hospital denials by dollar value stemming from incorrect coding.
But here’s what people often overlook: the same coding data that determines whether a claim receives payment also influences your ability to negotiate better rates.
When contract optimization specialists build rate cases for payer negotiations, they rely on your data—CPT code volumes, claim patterns, and reimbursement histories. If coding errors pollute that data, they weaken your negotiating position before you even begin. Clean coding data gives you leverage.
The Three Ways Coding Impacts Contract Optimization
1. Data Quality for Rate Negotiations
Payers scrutinize your coding patterns during contract renewals. They’re looking at:
- Which procedures you perform most frequently
- How consistently you code similar cases
- Whether your documentation supports your code selection
- Your historical denial and audit patterns
Payers are using tighter edits, AI-driven audits, and value-based contracts, so the financial impact of coding errors is multiplying. When you approach a payer with a request for higher reimbursement rates, they’ll examine whether you’ve historically coded correctly. Patterns of over-coding or under-coding raise red flags that complicate negotiations.
2. Denial Rates Signal Operational Health
Nearly 40 percent of healthcare organizations report their claims are denied at least 10 percent of the time with rates continuing to climb. Your denial rate tells payers whether you’re a reliable partner or an administrative burden.
High denial rates suggest:
- Poor documentation practices
- Inadequate staff training
- Outdated code sets or reference materials
- Misalignment between clinical and billing teams
When negotiating contracts, payers view high-denial practices as higher-risk. They may offer less favorable terms or demand more stringent documentation requirements.
3. Missing Revenue You Haven’t Even Captured
Before negotiating better rates, you need to ensure you’re capturing the rates you already have. Inaccurate coding can lead to missing charges, resulting in lost revenue for organizations, with many practices leaving money on the table through under-coding.
Consider this: if you’re only capturing 85% of the revenue you’re entitled to under current contracts, negotiating a 10% rate increase only gets you to 93.5% of what you could be earning. Fix the coding first, then negotiate.
How to Know If Your Coding Is Undermining Your Contracts
Here are the warning signs that coding issues may be costing you more than just denied claims:
- You can’t produce reliable utilization reports by CPT code
If your practice management system can’t easily show you which procedures you perform most frequently and at what volumes, your data isn’t negotiation-ready.
- Your denial rate exceeds 10%
This signals systemic issues that payers will notice. Data revealed that 56% of coders failed audits in 2023, indicating widespread accuracy challenges across the industry.
- Your coders aren’t certified or haven’t had recent training
Coding systems like ICD-10, CPT, and HCPCS are regularly updated with new codes and revised guidelines, and failure to keep current can result in coding errors leading to claim denials or improper reimbursement.
- You frequently receive denials for “documentation doesn’t support code”
This indicates a disconnect between your clinical team and billing team—a gap that weakens negotiation positioning.
- Your contract management platform (if you have one) shows inconsistent patterns
The wide variance in how similar procedures are coded indicates accuracy problems that undermine data reliability.
Common Coding Issues That Undermine Contract Value
Documentation-Code Mismatch
The physician documents a complex encounter, but the coder selects a lower-level code because the documentation doesn’t explicitly meet coding requirements. Result: underpayment under current contracts and unreliable data for future negotiations.
Modifier Misuse
Missing or incorrect modifiers can trigger denials or inappropriate downcoding. Insurance companies require precise CPT, ICD-10, and HCPCS codes for processing claims, and mistakes such as incorrect codes, missing modifiers, or mismatched diagnosis and procedure codes can lead to denials.
Outdated Code Sets
Still using last year’s coding manuals? You’re generating errors that cost you both immediate reimbursement and long-term negotiating credibility.
Lack of Specificity
Using unspecified diagnosis codes when specific codes are available reduces the perceived complexity of your patient population, potentially impacting risk adjustment scores and value-based contract performance.

Strategic Sequencing: When to Address Coding vs. When to Negotiate Rates
This is where most practices make costly mistakes. They launch into contract negotiations without ensuring their data foundation is solid.
Address coding first if:
- Your denial rate exceeds 10%
- You lack consistent coding guidelines across providers
- Your coders aren’t certified or haven’t received recent training
- You can’t produce reliable utilization data by CPT code
- Your documentation frequently doesn’t support the codes billed
Focus on contract negotiation if:
- Your denial rate is below 5%
- You have clean, auditable coding practices
- Your rates haven’t increased in 3+ years
- You can demonstrate consistent, appropriate coding patterns
- You have reliable data showing rate discrepancies vs. market benchmarks
Most practices need both, but sequencing matters. Attempting to negotiate without clean data wastes time and potentially damages payer relationships.
How Clean Coding Data Strengthens Negotiation Cases
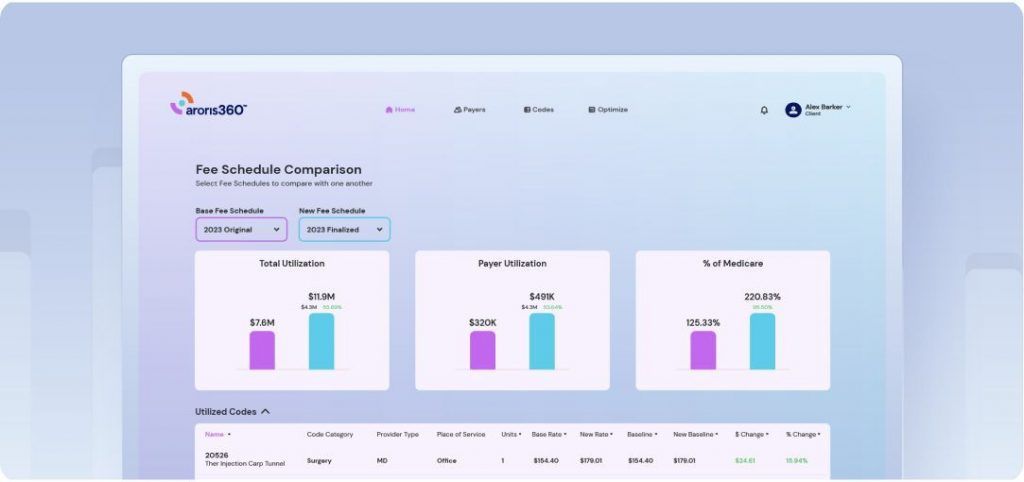
During contract analysis, optimization specialists examine specific payer-procedure combinations to identify rate improvement opportunities. They might discover that United Healthcare reimburses your highest-volume CPT codes 15% below Aetna’s rates for the same services.
To build that case effectively, you need:
- 12+ months of clean utilization data showing consistent code volume
- Documentation that supports complexity levels you’re reporting
- Low denial rates demonstrating payer acceptance of your coding
- Accurate contract fee schedule data to benchmark against actual payments
If your coding is inconsistent—sometimes billing 99214 for encounters that could support 99215, other times under-coding—the data becomes questionable. Payers can dismiss rate increase requests by questioning data validity.
This is why modern contract management platforms emphasize data visualization and accuracy validation before negotiation planning begins. They help identify both coding-related revenue opportunities and rate negotiation targets simultaneously.
A Dual-Lens Approach: Coding Optimization and Rate Negotiation
The most sophisticated practices don’t treat coding and contract optimization as separate initiatives. They address both by analyzing:
- CPT codes that are consistently under-coded based on documentation patterns
- High-volume procedures with significant rate variation across payers
- Procedures that generate frequent denials because of coding or authorization requirements
- Services eligible for higher reimbursement under alternative code sets
This comprehensive view ensures you’re maximizing revenue from every angle—capturing what you’re owed under current contracts while building the case for better rates.
Practical Steps for Medical Practices
1. Audit Your Current Coding Accuracy
Industry standard is 95% accuracy. If you’re below 90%, address this before approaching payers. Consider bringing in external auditors for an objective assessment.
2. Invest in Coder Education
Coding rules change annually. Budget for ongoing training, not just initial certification. Organizations like AAPC and AHIMA offer resources to keep coders current.
3. Implement Pre-Claim Scrubbing
Catch errors before submission. The cost of claim scrubbing software is far less than the cost of denials and appeals.
4. Track Denial Reasons by Code
Identify patterns. If certain CPT codes generate consistent denials, investigate whether it’s a coding issue, documentation problem, or contract term requiring clarification.
5. Build Documentation Templates
Make it easier for physicians to document in ways that support appropriate coding levels. Bridge the gap between clinical and billing teams through structured templates that capture required elements.
6. Generate Regular Utilization Reports
Before entering any contract negotiation, ensure you can produce clean reports showing your top 20 CPT codes by volume and revenue for each payer.
The Bottom Line
Medical reimbursement and coding accuracy isn’t separate from contract optimization—it’s the foundation. You can’t negotiate effectively from a position of data weakness.
If you’re considering a contract negotiation initiative, start by asking: “Is our coding data reliable enough to support our case?”
If the answer is uncertain, address coding quality first. This might mean:
- Conducting a comprehensive coding audit
- Investing in coder training and certification
- Implementing documentation improvement initiatives
- Deploying technology to catch errors before claim submission
If the answer is yes, you’re ready to explore what better rates could mean for your practice. Clean data serves as your strongest negotiating tool by showing payers exactly where rate improvements are justified and demonstrating your operational reliability.
Some practices need coding improvements before entering negotiations. Others have strong coding foundations ready to support aggressive rate optimization. The key is honest assessment of where you stand. Because in healthcare reimbursement, what you can prove matters more than what you deserve.