Running a medical practice means juggling dozens of moving parts simultaneously. From patient scheduling and billing to credentialing and compliance, practice management encompasses everything that keeps your doors open and your providers focused on patient care.
But here’s what successful practices understand: you can’t do everything well with limited resources. The practices that thrive make strategic decisions about which functions to handle in-house and where to seek specialized support. When critical revenue cycle components get deprioritized because you’re stretched too thin, they don’t just create isolated problems—they trigger cascading inefficiencies across your entire operation.
What Practice Management Actually Includes
Practice management isn’t a single function. It’s the intricate coordination of interconnected systems that together determine whether your practice runs smoothly or struggles constantly.
Clinical Operations
The foundation of patient care delivery includes appointment scheduling, patient registration with accurate insurance information, and exam room management that balances patient satisfaction with provider efficiency.
Revenue Cycle Management
This spans the entire payment journey from appointment scheduling through final collection:
- Insurance verification and prior authorization management
- Medical coding and claims submission
- Payment posting and reconciliation
- Denial management and appeals
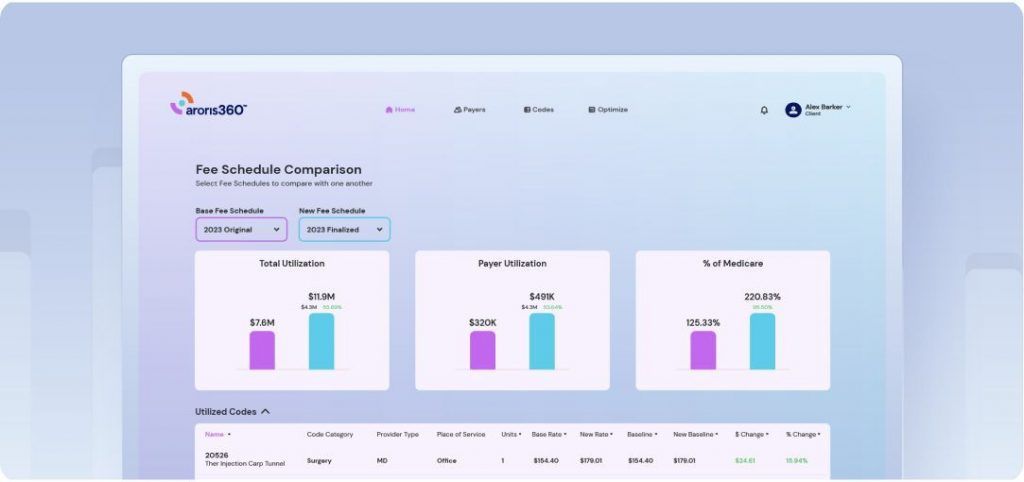
Contract Management and Rate Optimization
Often treated as separate from daily operations, this function directly determines how much you’re paid for services rendered. It includes negotiating payer contracts, maintaining organized contract repositories, monitoring whether payments match contracted rates, and preparing data-driven cases for renegotiations. Without this foundation, every other revenue cycle function operates blindly.
Provider Credentialing and Enrollment
This keeps your practice legally able to treat patients and bill insurance. The credentialing process can take three to six months for new providers—during which they see patients but you cannot bill insurance for their services. Miss a credentialing deadline, and claims get rejected until you resolve it.
Compliance and Regulatory Management
Multiple overlapping requirements protect your practice from penalties:
- HIPAA privacy and security compliance
- OSHA workplace safety requirements
- Medicare, Medicaid, and payer-specific policies
- State medical board licensure requirements
Each area requires ongoing documentation, staff training, policy updates, and audit preparedness.
Financial Management and Operations
This translates daily activity into business intelligence through accounts receivable and payable tracking, payroll processing, financial reporting by provider and service line, and budgeting for growth. Without clear financial visibility, you’re running your practice on intuition rather than data.
Human Resources and Staff Management
Building and retaining your team through hiring, onboarding, performance management, benefits administration, and scheduling. Staff turnover costs you in recruitment, training, lost productivity, and institutional knowledge that walks out the door.
Facilities, Technology, and Patient Experience
The physical and digital environment where care happens—from facility maintenance and medical equipment management to EHR systems and network infrastructure. Plus the patient-facing functions that shape perception and retention: front desk interactions, communication systems, patient education, and reputation management.
The Interconnected Reality
These areas don’t operate independently. When credentialing falls behind, billing can’t submit claims. When scheduling overbooks, clinical quality suffers and patient satisfaction drops. When contract rates aren’t monitored, revenue quietly erodes without anyone noticing until the financial damage is substantial.
This is why practice management feels overwhelming. It’s not one job. It’s orchestrating dozens of specialized functions simultaneously, each with its own requirements, deadlines, and consequences for failure.
Why Independent Practices Are Fighting for Survival
The scope of practice management responsibilities has become particularly crushing for independent medical practices. While large health systems can distribute these functions across specialized departments with dedicated staff, independent practices often expect administrators and small teams to handle everything.
The Financial Pressure Is Real
According to the American Medical Association, the top reason physicians sell their practices is that they need higher reimbursement rates to remain financially viable—rates they cannot negotiate effectively with insurers on their own.
The numbers tell the story:
- 63% of physicians report that cost structures and billing negatively impact their practice
- 38% of providers say increased payer issues have negatively impacted their revenue cycle
- 42% of physicians spend more than 10 hours per week on payer negotiations and related activities (AMA)
That last statistic deserves emphasis: nearly a quarter of a full-time workweek spent not on patient care, but on navigating insurance complexities.
The Data Gap Creates a Negotiating Disadvantage
According to Health Catalyst, 56% of healthcare executives cite data analytics as a major challenge in payer negotiations. Without organized contract data and payer performance metrics, practices enter negotiations blind—unable to prove underpayments or demonstrate their value.
The stakes are high. The Healthcare Financial Management Association documents a 300% disparity range in reimbursement rates for the same services across different payers. Two practices performing identical procedures might get paid wildly different amounts simply because one negotiated better rates. But independent practices often lack the bandwidth to even identify these gaps, let alone address them.
Why Consolidation Keeps Accelerating
These pressures directly fuel practice consolidation. Smaller practices don’t have the economies of scale to absorb mounting administrative costs efficiently. When you’re facing:
- New providers who can’t be credentialed for 3-6 months
- 10+ hours weekly spent on payer negotiations
- Revenue hemorrhaging through underpayments you can’t track
- Administrative costs that keep climbing
The appeal of joining a larger system that handles these burdens becomes undeniable.
The tragedy is that consolidation often doesn’t serve patients or communities well. Independent practices typically provide more personalized care, maintain stronger community connections, and offer more accessible services. But financial sustainability matters. You can’t serve your patients if you can’t keep your doors open.
The Hidden Cost of Trying to Do Everything In-House
Most practice administrators pride themselves on being resourceful problem-solvers who can handle anything thrown their way. That versatility is admirable—and often necessary in smaller practices where everyone wears multiple hats.
But there’s a difference between being versatile and being spread so thin that critical functions suffer. When your team is managing everything from patient scheduling to payer contract negotiations to credentialing to compliance, something inevitably gets less attention than it deserves.
Consider contract management specifically. Payer contracts now include hundreds of rate variations, modifier rules, bundling policies, and periodic updates that rarely get communicated clearly. Without active contract management, practices face:
Revenue leakage from underpaid claims – When negotiated rates don’t match what you’re actually receiving, you lose money on every encounter. Multiply that across thousands of claims, and the financial impact becomes substantial.
Wasted administrative hours – Staff spend hours reconciling payments, researching rate discrepancies, and filing appeals for underpayments they can’t easily prove. These hours add up, costing you both in payroll and opportunity cost.
Missed contract renegotiation opportunities – Without baseline rate data and payer performance metrics, your negotiating position weakens. You can’t advocate for better terms when you lack evidence of systematic underpayment.
Credentialing delays and gaps – Contract management and credentialing intersect constantly. When your contract data isn’t organized, credentialing processes slow down, delaying revenue from new providers or payers.
But contract management isn’t the only area where this pattern plays out. Billing and coding expertise, credentialing specialization, compliance monitoring, financial analytics—each of these domains has become complex enough that dedicating internal resources may not be the most efficient approach.
Why Administrative Overload Isn’t Inevitable
The phrase “administrative burden” gets thrown around so frequently in healthcare that it’s become white noise. But the overload your practice management team experiences isn’t an unavoidable cost of doing business—it’s often a symptom of trying to maintain expertise across too many specialized domains.
Think about what happens when your team handles everything internally:
- Every new regulation requires internal research and process updates
- Specialized tasks get performed by generalists who learned on the job
- Staff turnover means critical knowledge walks out the door
- Your practice administrator spends time on tactical execution instead of strategic planning
- Technology investments sit partially utilized because no one has time to master them
This isn’t a failure of your team. It’s a recognition that healthcare administration has become too specialized for small teams to maintain deep expertise everywhere.
Making Strategic Choices About External Support
Here’s the shift that separates struggling practices from thriving ones: recognizing which functions benefit from specialized external support versus which require in-house control.
Some functions need to stay in-house because they’re core to your practice identity and patient relationships. Patient scheduling, front desk operations, clinical workflows—these typically require intimate knowledge of your practice culture and immediate responsiveness.
But other functions—particularly those in the revenue cycle—often benefit from specialized expertise and dedicated focus. When you partner with specialists for specific components:
Your team focuses on higher-value work – Instead of your practice administrator spending hours researching payer contract terms, they can focus on strategic planning, staff development, and patient experience improvements.
You access specialized expertise – Professionals who focus exclusively on one domain (credentialing, contract negotiation, coding, compliance) maintain current knowledge that generalists can’t match.
You gain leverage and resources – Specialized partners often have relationships, data, and tools that individual practices can’t justify building internally.
Your financial performance improves – When experts handle revenue cycle components, you typically see measurable improvements that more than justify the investment.
The key is being selective and strategic. Not every function benefits from outsourcing. But the functions that directly impact revenue—contract management, specialized coding, credentialing, denial management—often deliver significant returns when handled by dedicated experts.
Investing in What Scales
Many practices resist seeking external support because it feels like admitting they can’t handle everything themselves. But this thinking misses the point entirely.
The strongest practice administrators aren’t the ones who do everything personally. They’re the ones who orchestrate resources—internal and external—to deliver the best outcomes for their practice.
Consider what happens when you offload specialized functions to experts:
- Your in-house team operates at the top of their capabilities
- You can scale operations without proportionally scaling overhead
- You access expertise that would be impossible to maintain internally
- Your practice administrator shifts from firefighting to strategy
This matters particularly for growth. Practices that try to scale by simply adding more generalist staff hit diminishing returns fast. The practices that grow sustainably build systems where specialized functions get specialized attention.
The Bottom Line
Effective practice management means making strategic decisions about where to invest resources and where to seek support. Not every operational challenge deserves the same approach.
The most successful independent practices aren’t the ones doing everything in-house and wearing their self-sufficiency as a badge of honor. They’re the ones that identified which functions benefit from specialized expertise—and made strategic decisions to access that expertise however it makes sense.
Whether that means technology investments, outsourced services, consulting partnerships, or specialized software, the principle remains the same: focus your internal resources where they matter most, and get strategic support for specialized functions that directly impact your financial sustainability.
Your practice administrator can’t be an expert in everything. They shouldn’t have to be.