Healthcare providers face financial pressures from all directions. Between rising operational costs, administrative burdens, and shifting reimbursement models, medical practices are constantly searching for ways to maintain financial sustainability. One often overlooked opportunity lies in fee schedule optimization – a strategic approach to analyzing and improving the rates paid by insurance companies for healthcare services.
Understanding fee schedules in healthcare
A fee schedule is a comprehensive list of services and procedures that a healthcare provider offers, paired with the corresponding payment amounts they will receive from insurance companies. These schedules serve as the financial backbone of medical practices, directly impacting revenue and sustainability.
Fee schedules vary significantly across different insurance companies, specialties, and geographic regions. What many providers don’t realize is that these schedules aren’t set in stone – they’re negotiable documents that present opportunities for revenue enhancement.
The impact of unfavorable fee schedules
Many healthcare organizations operate with fee schedules that haven’t been thoroughly analyzed or renegotiated for years. The financial consequences can be substantial:
- Reimbursement rates that fail to keep pace with inflation and rising practice costs
- Payment disparities of up to 300% for identical services across different payers
- Reduced profitability for high-volume procedures that form the core of your practice
- Unnecessary revenue leakage that compounds over time
A medical practice with $5 million in annual revenue could be leaving $500,000 or more on the table due to inefficient fee schedules. For larger organizations, this figure can reach into the millions.
Fee schedule analysis: The first step toward optimization
Before attempting to negotiate improved rates, providers need a clear understanding of their current fee schedule landscape. A comprehensive fee schedule analysis involves:
- Digitizing all contracts and fee schedules into a searchable, analyzable format
- Identifying your highest-volume CPT codes that drive the majority of revenue
- Benchmarking your rates against Medicare, regional averages, and other payers
- Calculating the revenue impact of rate discrepancies across your payer mix
- Prioritizing opportunities based on contract renewal dates and potential ROI
This analysis frequently reveals surprising insights. For example, a practice might discover that its highest-volume CPT codes are reimbursed at 20-30% below market rates by certain payers, while less common procedures are paid at or above market rates – creating an illusion of fair compensation while significantly underpaying for the most important services.
Strategies for negotiating fee schedules with insurance companies
Negotiating fee schedules with insurance companies requires preparation, persistence, and a strategic approach. Here are proven strategies to enhance your negotiating position:
1. Leverage data-driven insights
Insurance companies respond to well-documented cases supported by objective data. When approaching fee schedule negotiation, present clear visualizations comparing your rates to market benchmarks. Focus on specific high-volume CPT codes where the disparity is greatest. Demonstrate the value your practice brings to the payer’s network through quality metrics. Calculate the total revenue impact of proposed changes to show reasonableness.
2. Know your value to the payer
Your negotiating position is strengthened when you understand your importance to the insurance company’s network. Document the number of their members you serve. Highlight any unique services or specialties you provide in your region. Emphasize quality metrics, patient satisfaction scores, and cost-efficiency data. Be prepared to discuss your participation in other networks as alternatives.
3. Adopt a long-term approach
Fee schedule negotiation isn’t a one-time event but an ongoing process. Establish a regular cadence for contract reviews and negotiations. Prioritize payers based on contract renewal dates and revenue impact. Take a phased approach, focusing on the most impactful codes first. Build relationships with payer representatives beyond just negotiation periods.
4. Consider alternative payment models
While fee for service remains dominant, exploring alternative payment models can sometimes yield stronger results. Explore options for bundled payments for common episodes of care. Consider sliding fee schedules that adjust based on volume thresholds. Evaluate pay-for-performance provisions that reward quality outcomes. Assess capitation models for appropriate patient populations.

Practical steps to implement fee schedule optimization
For providers ready to pursue fee schedule optimization, here’s a practical roadmap:
Step 1: Gather and organize your data
Begin by collecting all payer contracts, fee schedules, and at least 12 to 24 months of claims data. This provides the foundation for your analysis and strategy development.
Step 2: Conduct a thorough fee schedule analysis
Analyze your data to identify which CPT codes generate the most revenue for your practice. Determine how your reimbursement rates compare across different payers. Pinpoint where the largest rate disparities exist compared to market benchmarks. Identify which payers represent the greatest opportunity for improvement.
Step 3: Develop a negotiation strategy
Create a customized approach for each payer based on contract renewal timelines. Consider potential revenue impact, your leverage in their network, and historical negotiation patterns.
Step 4: Execute and document negotiations
When engaging with payers, present clear, data-backed proposals focusing on a specific fee schedule for CPT codes. Document all communications and counteroffers. Remain professional and focused on any mutual benefits. Be prepared for multiple rounds of discussion.
Step 5: Implement and monitor results
After negotiations, update your practice management system with new rates. Verify that new rates are being correctly applied to claims. Track the financial impact of rate changes. Document the process for future negotiation cycles.
Real-world results from fee schedule optimization
Healthcare organizations that implement strategic fee schedule optimization typically see significant financial improvements. Here are a few examples:
- An orthopedic group in the Midwest identified a proposal from United Healthcare that appeared to offer an 8% fee schedule increase but would have actually resulted in a 1.12% revenue decrease. After analysis and negotiation, they secured a true 8.08% increase, substantially impacting their bottom line.
- A behavioral health provider was able to convert a proposed 8% rate decrease into a 12.9% increase by using objective market data and strategic negotiation techniques – representing more than a twenty-point swing in reimbursement rates.
- A multi-specialty medical physician fee schedule was optimized across multiple payers, achieving an average 10.5% rate increase, even with insurers that had previously claimed their rates were “non-negotiable.”
Overcoming common challenges in fee schedule negotiation
Despite the clear benefits, many providers encounter obstacles when attempting to optimize their fee schedules. Some of these obstacles include:
Time and resource constraints
Most practice administrators report spending more than 10 hours per week on payer-related activities, leaving limited bandwidth for contract analysis and negotiation. This often results in automatic renewals of suboptimal contracts simply due to lack of time.
Data limitations
Without access to comprehensive market benchmarking data, providers negotiate from a position of information disadvantage. Payers have visibility into rates across their entire network, while providers see only their own contracts.
Negotiation expertise
Effective negotiation requires specialized skills and experience that many healthcare administrators haven’t had the opportunity to develop, particularly when facing seasoned insurance company representatives.
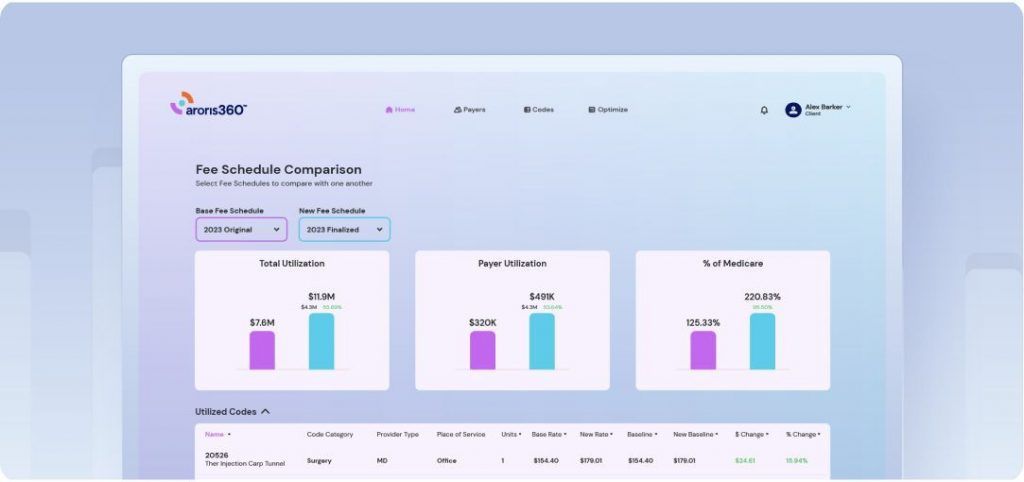
Aroris360, our proprietary contract management platform, can help. Learn how.
The path forward: Making fee schedule optimization a priority
For healthcare providers committed to financial sustainability, fee schedule optimization represents a significant opportunity to improve revenue without increasing patient volume or cutting costs. By treating payer contracts as strategic assets rather than administrative burdens, practices can unlock hidden revenue potential while building stronger, more equitable payer relationships.
The key is approaching fee schedule management systematically, supported by robust data analysis and negotiation expertise. Whether developed internally or through specialized partners, these capabilities are becoming essential components of healthcare financial management.
As reimbursement pressures continue to intensify, providers who proactively optimize their fee schedules will gain a meaningful financial advantage over those who continue to accept whatever rates insurers offer. The difference could determine which practices thrive instead of just survive in tomorrow’s healthcare landscape.
Ready to optimize fee schedules? Get a demo of Aroris360 now.