Healthcare providers face an increasingly complex web of payer relationships, governed by unique contract terms, reimbursement rates, and compliance requirements. With more than 42% of doctors spending over 10 hours a week on payer negotiations, the need for robust contract management systems has never been more critical.
What is contract management in healthcare? It’s the systematic approach to creating, executing, and analyzing contracts with payers, vendors, and partners to maximize value while minimizing risk. The right healthcare contract management software doesn’t just store documents—it transforms how your organization approaches payer relationships and revenue optimization.
Here are the ten essential features that separate truly effective contract management systems from basic document storage platforms.
1. Comprehensive Payer Data Integration
Effective contract management in healthcare is dependent on successful data integration. Quality data integration should help track provider payment patterns and performance. Your contract management platform should seamlessly connect with multiple data sources, including claims systems, revenue cycle management platforms, and payer transparency databases.
This integration enables real-time visibility into the performance of payer contracts, allowing you to identify discrepancies between contracted rates and actual payments. Without this feature, even the best contract management software becomes little more than an expensive filing cabinet.
Look for systems that can automatically import and reconcile provider payment data from various sources, creating a unified view of your payer relationships. This capability is essential for payer contract management because it provides the analytical foundation needed for successful contract negotiation.
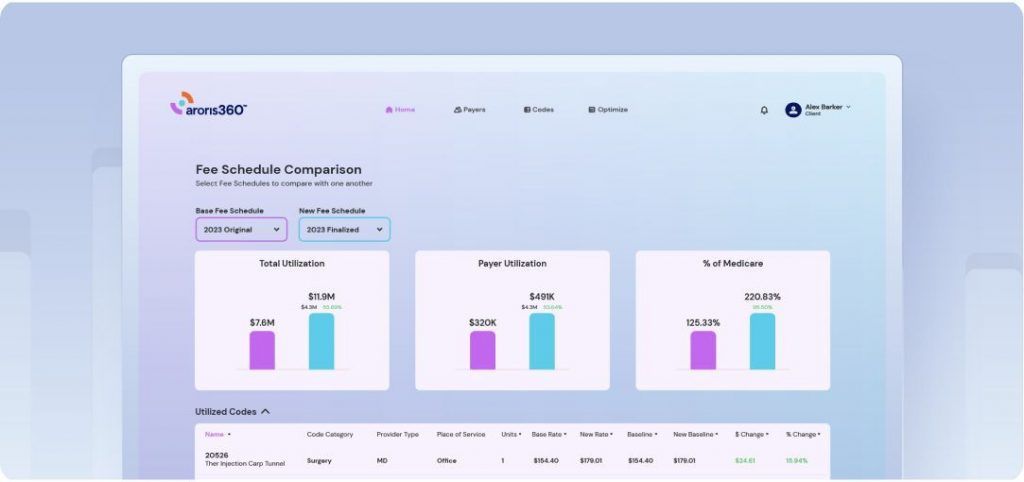
2. Advanced Contract Optimization Analytics
Effective payer contract management software requires more than just storing contract terms—it demands sophisticated analytics that reveal contract optimization opportunities. Your contract management system should provide detailed performance metrics, trend analysis, and market benchmarking capabilities.
The best healthcare contract management software includes features like:
- Revenue variance analysis comparing contracted vs. actual provider payment amounts
- Payer performance scorecards tracking payment speed and denial rates
- Market benchmarking against regional and national standards for payer contracts
- Predictive analytics identifying contracts due for contract negotiation
These analytics transform raw contract data into actionable insights, enabling data-driven decisions about which payer contracts to prioritize for renegotiation and which contract terms offer the greatest contract optimization potential.
3. Automated Renewal and Provider Enrollment Management
Manual tracking of contract renewal dates and provider enrollment deadlines creates unnecessary risk for healthcare providers. A robust contract management system should include automated alerts and workflow management to ensure nothing falls through the cracks during the contract negotiation process.
This feature becomes particularly critical for contracts and negotiations where organizations may manage hundreds of different agreements simultaneously. The contract management tools should track:
- Contract expiration dates with customizable alert timelines
- Provider enrollment compliance milestone deadlines
- Performance review requirements for payer contracts
- Amendment and addendum tracking
Automated workflow capabilities ensure the right stakeholders receive timely notifications, preventing costly oversights that could impact provider payment or compliance status.
4. Real-Time Payer Contracts Performance Monitoring
Your contract management software should provide continuous monitoring of payer contracts performance against established baselines. This goes beyond simple reporting to include real-time alerts when performance metrics fall outside acceptable ranges.
For payer contract management software, this means tracking metrics like:
- Claims payment timeliness affecting provider payment
- Denial rates by procedure code
- Underpayment frequency
- Prior authorization approval rates
Real-time monitoring helps you manage payer contracts better, letting you fix problems before they affect provider payments.
5. Secure Document Repository with End to End Contract Management Process Support
While analytics drive strategy, effective contract management in healthcare still requires robust document management capabilities. Your contract management solution should provide secure, searchable storage that supports the end to end contract management process.
Essential document management features include:
- Centralized storage with role-based access controls
- Advanced search capabilities across payer contracts content
- Automated version tracking and change history
- Integration with electronic signature platforms for contract negotiation
- Audit trails for compliance purposes
This foundation supports the entire contract management process while ensuring sensitive information remains secure and accessible to authorized users.
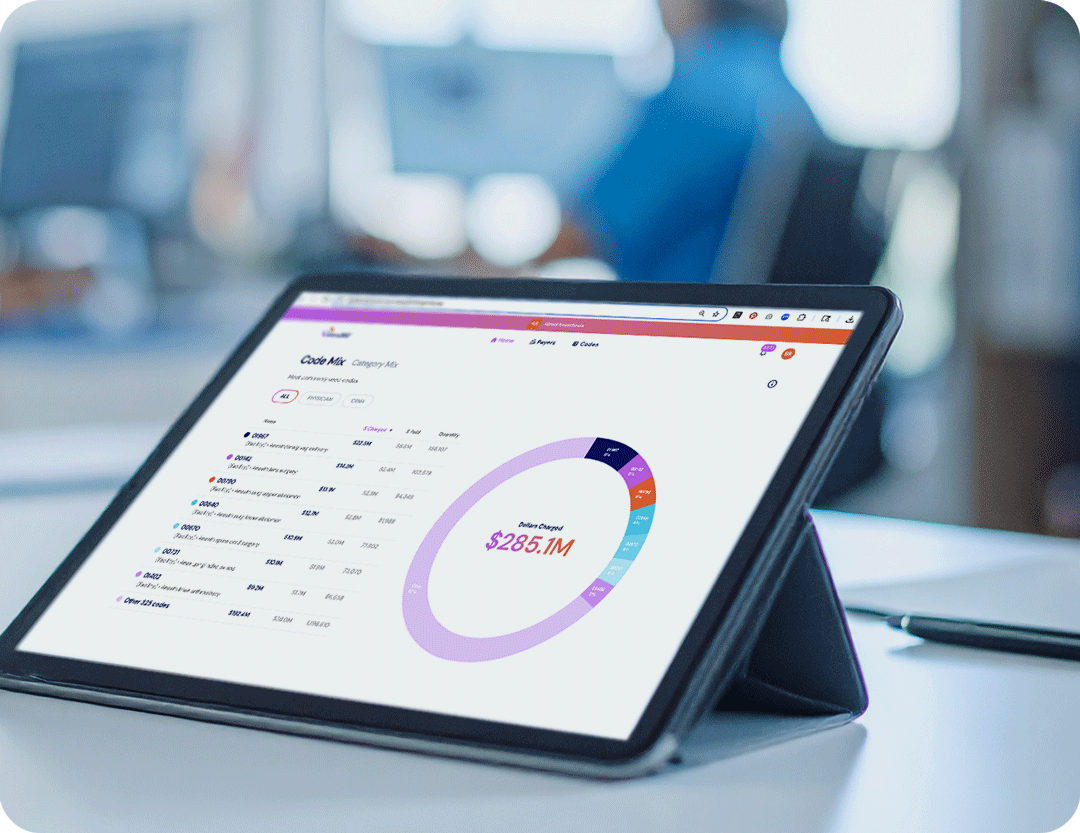
6. Customizable Reporting and Healthcare Consulting Insights
Different stakeholders need different views of payer contracts performance data. Executives want high-level summaries, while contract administrators need detailed operational metrics. Your software for contract management should offer customizable dashboards and reporting capabilities that serve all user types.
Effective reporting features include:
- Executive-level provider payment performance summaries
- Operational dashboards for daily contract management activities
- Detailed analytics for contract negotiation preparation
- Automated report generation and distribution
- Custom report building capabilities for healthcare consulting needs
This flexibility ensures all stakeholders have access to relevant information in formats that support their contract management process decisions.
7. Integration with Revenue Cycle and Provider Enrollment Systems
Contract management for healthcare cannot operate in isolation from broader revenue cycle operations. Your contract management platform should integrate seamlessly with existing revenue cycle management systems, provider enrollment databases, electronic health records, and financial reporting tools.
This integration enables:
- Automated validation of claims against payer contracts terms
- Real-time identification of provider payment discrepancies
- Streamlined denial management workflows
- Comprehensive revenue cycle analytics for contract optimization
Without proper integration, even sophisticated contract management systems in healthcare may fail to deliver their full potential value.

8. Collaborative Contract Negotiation Workflow Management
Healthcare contract management process involves multiple stakeholders across different departments. Your contract management tools should support collaborative workflows that enable efficient communication and task management during contract negotiation.
Key workflow features include:
- Task assignment and tracking capabilities for contract negotiation
- Commenting and annotation tools for payer contracts review
- Approval workflow automation
- Integration with email and communication platforms
- Mobile access for remote contract management collaboration
These capabilities ensure all stakeholders can participate effectively in the end to end contract management process, regardless of their location or role.
9. Compliance Monitoring and Contract Negotiations Risk Assessment
Payer contracts operate within a complex regulatory environment. Your hospital contract management software should include built-in compliance monitoring and risk assessment capabilities that help identify potential issues before they become problems during healthcare payer contract negotiations.
Essential compliance features include:
- Regulatory requirement tracking for provider enrollment
- Risk scoring for payer contracts terms
- Compliance deadline management
- Audit trail maintenance for contract negotiation activities
- Integration with compliance management systems
For contract management in healthcare, this includes monitoring for anti-kickback statute compliance, Stark Law requirements, and other healthcare-specific regulations that affect provider payment.
10. Scalable Architecture and Healthcare Consulting Support
As your organization grows, your contract management tools must scale accordingly. Look for contract management systems in healthcare built on modern, scalable architectures that can accommodate increasing data volumes and user counts without performance degradation.
Additionally, evaluate the vendor’s healthcare consulting and support capabilities:
- Implementation and training services for contract management process
- Ongoing technical support for payer contract management software
- Regular system updates and enhancements
- User community and knowledge resources
- Data migration assistance for existing payer contracts
The end to end contract management process requires not just good software for contract management, but also reliable vendor partnership to ensure long-term success.
Making the Right Choice for Your Organization
Selecting the right contract management solution requires careful evaluation of your organization’s specific needs, existing technology infrastructure, and strategic objectives for contract optimization. The contract management software that works best for a small practice may not meet the needs of a large health system managing complex healthcare payer contract negotiations.
Consider conducting a thorough needs assessment that includes input from all stakeholders who will interact with the contract management system. This assessment should evaluate current pain points with payer contracts, desired outcomes for provider payment optimization, and integration requirements with existing systems.
Remember that implementing contract management systems is not just a technology decision—it’s a strategic investment in your organization’s financial future. The right contract management platform can transform payer contracts from administrative burdens into strategic advantages for contract optimization.
The Bottom Line
Effective payer contract management software serves as the foundation for optimizing payer relationships and maximizing provider payment potential. By focusing on these ten essential features, healthcare providers can select contract management systems that not only meet today’s needs but also support future growth and success in healthcare payer contract negotiations.
The complexity of modern healthcare contracting demands sophisticated contract management tools that go beyond basic document storage. Organizations that invest in comprehensive contract management systems position themselves to navigate payer contracts more effectively, identify contract optimization opportunities more quickly, and maintain compliance more reliably.
As the healthcare landscape continues to evolve, those organizations with robust contract management capabilities will be best positioned to thrive in an increasingly competitive environment. The end to end contract management process becomes a competitive advantage when supported by the right contract management solution.