One critical component that directly impacts financial success in medical practices often gets treated as administrative overhead: medical credentialing. Understanding credentialing as both a quality assurance mechanism and a strategic revenue tool can transform how medical practices approach payer relationships and contract optimization.
What Is Medical Credentialing?
Medical credentialing is a comprehensive verification process that confirms healthcare professionals’ qualifications, training, licenses, and competency. This rigorous vetting ensures practitioners meet industry standards before delivering patient care and serves as the gateway between healthcare providers and insurance networks.
Without proper credentialing, providers cannot participate in insurance networks, severely limiting their patient base and revenue potential. Medical credentialing impacts healthcare professionals—physicians, nurse practitioners, therapists, and specialists—across multiple practice settings.
The Three Stages of Medical Credentialing
The credentialing process involves distinct stages, each requiring meticulous attention to detail and adherence to specific timelines:
1. Initial Credentialing
Provider credentialing begins with comprehensive document collection and primary source verification. Healthcare providers must submit education history, training records, work experience, licensure, certifications, malpractice insurance, and professional references. Credentialing specialists contact original sources—medical schools, licensing boards, and certification agencies—to confirm all credentials.
This stage includes background screening for malpractice claims, disciplinary actions, and criminal records, followed by committee review to evaluate qualifications against established standards.
2. Ongoing Monitoring and Recredentialing
Providers typically undergo re-credentialing every 2-3 years to maintain network status. This continuous monitoring ensures providers maintain current licenses, continuing education credits, and malpractice coverage while tracking compliance requirements and upcoming expirations.
3. Specialty Credentialing and Network Enrollment
Specialty credentialing occurs when providers need approval for specific procedures, advanced treatments, or specialized services beyond basic network participation. Once credentialed, providers undergo enrollment with insurance companies to become in-network providers, each with unique requirements and processing timelines.

Types of Healthcare Credentialing
Different credentialing types serve specific purposes and open various revenue opportunities:
Hospital Privileging
- Grants providers permission to practice specific services within healthcare facilities based on their qualifications and experience
Insurance Network Credentialing
- Enables providers to join insurance networks and meet payer quality and payment standards
Medicare/Medicaid Credentialing
- Ensures providers meet federal requirements for government programs with specific compliance standards
Specialty Board Certification
- Confirms provider expertise in particular medical specialties through additional training and examination
The Critical Link Between Medical Credentialing and Revenue Optimization
Here’s where most practices miss a crucial opportunity. Credentialing isn’t just about compliance—it’s about positioning for financial success and strengthening payer contract management.
Negotiating Leverage Through Multi-Network Participation
Providers who maintain current credentialing across multiple networks have greater leverage during contract negotiations. This multi-network participation demonstrates market value and provides alternatives that strengthen negotiating positions during payer contract management discussions.
Strategic Timing with Contract Renewal Cycles
Coordinating credentialing activities with contract renewal cycles allows practices to leverage new credentials and expanded services during negotiations. This strategic alignment maximizes opportunities for improved contract terms and enhanced reimbursement rates.
Access to Enhanced Payment Models
Many value-based care programs and quality incentive opportunities require specific credentialing elements that traditional fee-for-service arrangements may not emphasize. Comprehensive credentialing strategies position practices for these enhanced payment opportunities while ensuring access to all available reimbursement rates for specialized procedures.
How Medical Credentialing Delays Impact Financial Performance
Understanding the financial implications of credentialing delays is crucial for practice management:
Direct Revenue Loss
A provider generating $50,000 monthly in collections who experiences a 90-day credentialing delay represents $150,000 in lost revenue during that period. This lost income cannot be recovered retroactively, as most payers do not reimburse for services provided before credentialing completion.
Operational Cost Continuation
While credentialing stalls, practices continue paying provider salaries, benefits, and associated overhead costs without corresponding revenue generation. This creates a double financial burden that can strain practice resources and force reliance on credit lines.
Patient Access and Satisfaction Impact
Credentialing delays create significant patient experience challenges:
- Reduced Appointment Availability: When new providers cannot see insured patients, existing providers face increased scheduling pressure
- Network Adequacy Issues: Delays limit patient access to care within their insurance networks
- Continuity of Care Disruptions: Gaps between departing and replacement providers impact health outcomes and satisfaction
Common Medical Credentialing Challenges
Despite its importance, the credentialing process presents several obstacles:
- Time-Intensive Process: Credentialing often requires 60 to 180 days to complete, delaying provider onboarding and revenue generation
- Complex Documentation Requirements: Varying standards across different organizations, with each payer potentially requiring unique information or formats
- Ongoing Maintenance: Tracking and renewing credentials regularly requires consistent administrative attention and resource allocation
- Balancing Efficiency with Compliance: Organizations must avoid delays while ensuring they meet all quality and regulatory standards
How Professional Medical Credentialing Services Add Value
Specialized credentialing companies offer expertise that individual practices often cannot achieve independently:
Administrative Efficiency
- Collect and organize comprehensive documents in secure, accessible repositories
- Submit applications to multiple entities simultaneously with proper formatting
- Track application status and follow up promptly with payers
- Handle re-credentialing requirements through proactive renewal processes
Strategic Benefits
- Reduced Administrative Burden: Staff can focus on patient care rather than paperwork
- Faster Approval Timelines: Specialists navigate payer systems and requirements effectively
- Fewer Denials: Complete, accurate applications meet all requirements before submission
- Revenue Protection: Prevents delays in reimbursement that occur when credentialing issues arise
- Compliance Assurance: Keeps practices updated with constantly changing regulatory requirements
Maximizing Revenue Through Strategic Medical Credentialing
Effective credentialing strategies impact payment rates and terms in two key ways:
Payment Processing Efficiency
Proper credentialing ensures accurate provider identification in billing systems, reducing claim denials and payment delays. Complete credentialing that includes all relevant specialties and service locations minimizes billing complications and accelerates revenue collection.
Market Positioning for Contract Negotiations
Credentialing completeness influences participation in higher-paying contracts and specialized programs. Providers with robust credentialing profiles can pursue more selective payer relationships and negotiate from positions of strength.
The Role of Healthcare Consulting in Credentialing Strategy
Healthcare consulting firms bring valuable expertise to both credentialing and contract optimization initiatives. These consultants understand how credentialing impacts overall payer relationships and can develop integrated strategies that support long-term financial objectives. Professional consultants provide objective evaluations of credentialing return on investment, helping practices prioritize efforts toward payer contracts offering the greatest revenue potential. This strategic approach ensures optimal resource allocation and maximizes the impact of credentialing investments.
Choosing the Right Credentialing Partner
When selecting credentialing support, consider these essential factors:
- Specialty Experience: Look for partners with significant experience in your specific medical field
- Payer Relationships: Ensure they maintain strong relationships with major insurance companies
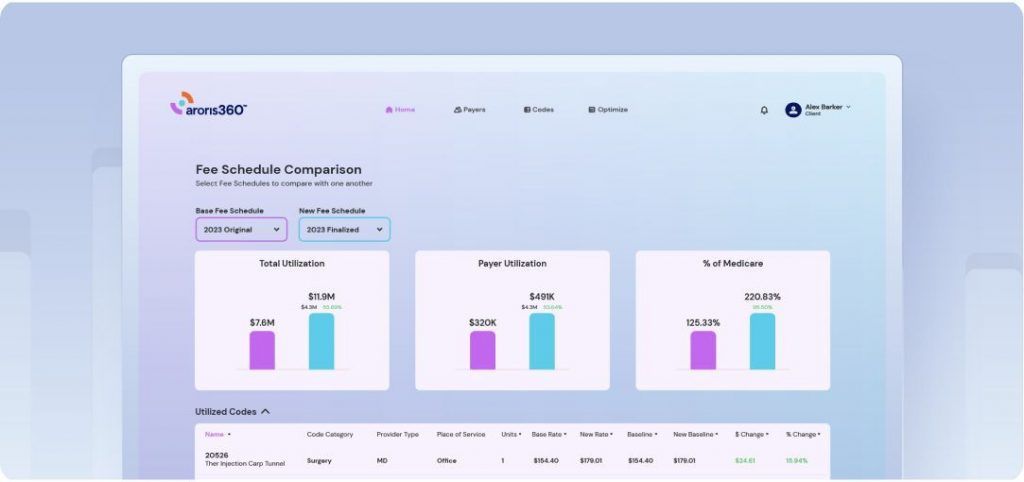
- Technology Solutions: Evaluate their systems for transparent, real-time reporting capabilities
- Communication Practices: Assess their responsiveness for timely credentialing updates
- Track Record: Review their success with similar organizations
Future-Forward Medical Credentialing Strategies
Progressive organizations are transforming credentialing from administrative necessity to strategic advantage through:
- Digital Workflows: Implementing paperless solutions that reduce errors and accelerate processing
- Data Integration: Connecting credentialing with billing, scheduling, and electronic health records
- Proactive Monitoring: Developing alert systems for upcoming expirations and compliance issues
- Performance Analytics: Using data to identify bottlenecks and optimize credentialing workflows
- Technology Integration: Leveraging advanced systems for streamlined processes and real-time status updates
The Bottom Line
Medical credentialing represents far more than regulatory compliance—it’s the foundation for successful payer relationships and optimal contract terms. Healthcare providers who recognize this connection and invest in comprehensive credentialing strategies position themselves for sustained financial success.
The integration of strategic credentialing with contract optimization creates powerful synergies that benefit both immediate revenue goals and long-term practice growth. Rather than viewing credentialing as a necessary burden, successful practices embrace it as a strategic foundation for financial optimization.
Success in modern healthcare requires seeing credentialing not as a compliance checkbox, but as a revenue optimization tool. Providers that adopt this perspective will find themselves better positioned to navigate complex payer relationships and maximize their reimbursement potential.